- Spine Surgeon
- Spine
- Robotic Surgery
- Diseases
- Treatments
- News & Media
- Contact
Disc Disease
What is Lumbar Disc Disease? Back Pain – Low Back Pain
Disc disease, or disc degeneration, is a condition caused by the degeneration of the intervertebral disc and the symptoms that arise from it. Disc degeneration is a natural process that, in many cases, does not present any symptoms. For example, by the age of 50, radiological findings of disc disease are expected in more than 50% of individuals.
Genetics play a significant role (similar to how skin aging affects the appearance of wrinkles), but environmental factors also contribute, such as heavy lifting, exposure to vibrations, smoking, etc. The intervertebral discs have a limited ability to heal from potential injuries due to the small number of cells inside the disc and the lack of blood vessels in the area (similar to the meniscus in the knee).
What are the Symptoms?
Pain is primarily localized in the lower back (low back pain – lumbago) and may radiate to the buttocks and the back of the thighs, reaching just above the knees but not extending to the foot. Symptoms worsen when sitting or standing/walking for extended periods and improve when lying down. Movement of the lower back (lumbar spine) is limited and painful.
The patient does not find relief by bending forward; in fact, this may worsen the pain due to the increased pressure inside the disc. During examination, sensation, mobility, and reflexes are usually normal.
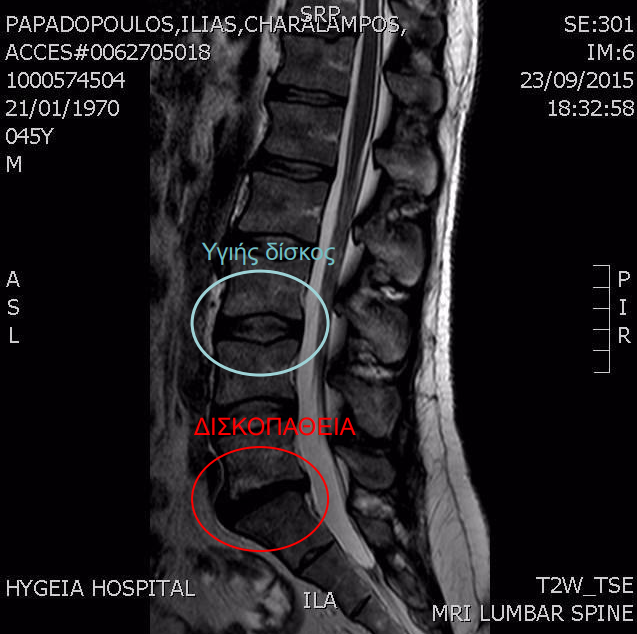
MRI scans show disc degeneration, including a reduction in disc height and changes in its signal (the disc appears black instead of white, as shown in Figure 1). However, these findings are not exclusive to symptomatic individuals, as they are commonly seen in asymptomatic patients of all ages.
Treatment – Management: Is Surgery Necessary? Medications – Exercises – Physiotherapy
Treatment is primarily conservative. In the acute phase, when pain is intense and interferes with daily activities, the following measures are recommended:
- Lumbar support belt (a standard lumbar support belt is sufficient).
- Heat therapy (some individuals may benefit from cold therapy, but heat packs are generally recommended).
- Medications: anti-inflammatory drugs, painkillers (simple and opioid-based), and medications for chronic pain (Gabapentin, Pregabalin, etc.). No injections!
- Physiotherapy (early application of physiotherapy can be very effective for severe pain).
Avoid
- Prolonged bed rest in the same position.
- Injections
- Extreme alternative treatments (e.g., hitting with a hammer, etc.). Acupuncture, for example, can be highly beneficial, whereas chiropractic treatment may sometimes be harmful. Chiropractic adjustments should only be performed with a thorough understanding of lumbar pathology (MRI scan required). While various treatments may have relative success, classic physiotherapy is the most effective.
Chronic Phase Management of Disc Disease – Importance of Exercise
In the chronic phase of disc disease, regular exercise is essential:
- Aerobic exercise such as walking, running, swimming, cycling, elliptical training, or any activity that increases heart rate, ideally 2-3 times per week.
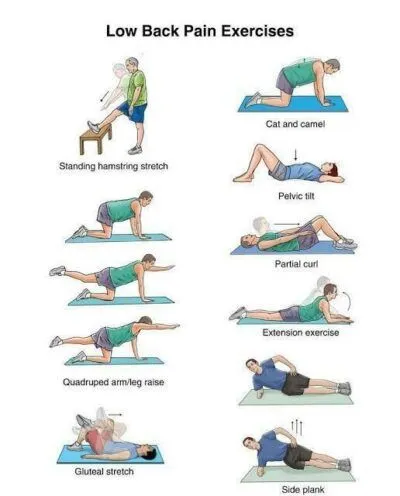
- Strengthening the spine through abdominal and back muscle training is also crucial (Figure 2). Pilates has been found to be the most effective exercise, as it strengthens the core muscles isometrically (without excessive movement that stresses the spine) and incorporates leg stretches that significantly help with low back pain.
Minimally Invasive Procedures
The most common minimally invasive intervention is a cortisone injection, either into the epidural space or into the spinal joints. However, for lower back pain alone, cortisone injections are less effective than they are for leg pain caused by a herniated disc.
Other minimally invasive procedures involve destroying the painful disc tissue to make it painless. This can be done through:
- Heat application (IDET, RF, LASER).
- Injection of substances (Discogel).
- Mechanical destruction of the disc in an attempt to destroy the nerve fibers within the painful disc, thereby reducing pain.
Unfortunately, none of these methods have been proven effective. In some cases, pain may worsen after the intervention.
A particular mention should be made regarding Discogel injections inside the disc. In Greece, Discogel is overused despite a lack of scientific evidence supporting its effectiveness (PubMed research). An even more outdated treatment is laser disc procedures, which have been banned in the U.S. due to their potential to worsen back pain.
In conclusion, apart from traditional cortisone injections, none of the minimally invasive disc procedures have proven their effectiveness, meaning their application is not justified despite their low risk.
Spinal Fusion – Disc Reconstruction
When conservative treatment fails and pain persists, spinal fusion is the only solution. If disc disease affects one or two levels, surgery yields excellent results. However, a small percentage of patients do not experience pain relief after fusion surgery, making proper patient selection crucial.
Key criteria for surgical candidates:
- Patients must have failed conservative treatment, which includes at least six months of consistent exercise therapy.
- Patients with disc disease affecting three or more levels are not candidates for surgery.
In spinal fusion, the painful disc is removed, and the vertebrae are fused using bone grafts and screws to eliminate movement at that level. MRI scans help identify the affected disc, but no test can definitively confirm that a specific disc is the sole source of pain. Discography, once used in the past, is now considered unreliable.
A successful fusion requires the vertebrae to permanently bond and eliminate movement. This is achieved using anterior-posterior spinal fusion, involving disc removal, bone graft placement, and posterior screw stabilization.
Factors influencing success:
- Careful patient selection.
- Successful spinal fusion (bone formation at the disc site).
The surgical approach (whether from the back or abdomen) and the incision size (traditional or minimally invasive surgery) do not significantly impact the final outcome, as long as the fusion is successful. Navigation-assisted and robotic surgery, while promising, do not show a significant advantage for small fusions (1-2 levels).
Spinal Fusion Complications
Spinal fusion has a low complication rate, but possible issues include:
- Wound infection.
- Deep vein thrombosis (DVT) or pulmonary embolism.
- Neurological damage (nerve injury or paralysis is extremely rare and minimized with intraoperative neuromonitoring).
Specific complications include:
- Fusion failure, leading to screw loosening or breakage.
- Adjacent segment degeneration, due to increased load transfer to the nearby level or natural degeneration.
Total Disc Replacement
Total disc replacement in the lumbar spine has not gained the same acceptance as in the cervical spine. The goal of artificial discs is to remove the diseased disc while preserving motion. Potential advantages include protecting adjacent discs from wear and maintaining spinal movement.
However, FDA studies (IDE trials) show no significant difference in pain relief between total disc replacement and spinal fusion. Additionally, many artificial discs become immobile (“ankylosed”) within a decade.
Moreover, in cases of failed lumbar disc replacement, revision surgery is extremely difficult, if not impossible


